What is sleep apnea?
Sleep apnea is a sleep disorder that occurs when someone’s breathing is interrupted during sleep. Interrupted can mean completely stopping breathing or having a hard time breathing. Some people with untreated sleep apnea stop breathing repeatedly during sleep and this can be measured by having a polysomnograph (PSG) sleep test or a home sleep test (HST). The sleep physician that reads and interprets the sleep test will diagnose the patient with sleep apnea depending on what the Apnea Hypopnea Index (AHI.) A normal AHI is 5 or less, mild is from 5-15, moderate is from 15-30 and anything over 30 is severe.
Who is at risk and what are some symptoms for sleep apnea?
There are more than 200,000 cases diagnosed per year in the US alone. 1 in 5 adults have mild sleep apnea and 1 in 15 adults have moderate to severe sleep apnea. This is very prevalent and most people who have it do not even know that they do. It is rare for ages 0-2, less common for ages 3-18, more common for ages 19-40 and very common from ages 41-60+. It is more prevalent in males than females but females are more likely to have it during menopause. Common risk factors include obesity, diabetes, A-fib, hypertension, familial history of Sleep apnea, GERD or acid reflux, history of heart attacks, strokes, individuals with a large tongue or tonsils, sinusitis, large neck size, smokers and alcohol users. Symptoms of sleep apnea include but are not limited to loud or frequent snoring, silent pauses in breathing, choking or gasping sounds, daytime sleepiness or fatigue, unrefreshing sleep, insomnia, morning headaches, depression, loss of energy, lack in interest of hobbies, dry mouth or sore throat in the morning, irregular heart beat, and trouble concentrating or remembering things. Untreated sleep apnea increases the risk of heart attacks, hypertension, congestive heart failure, stroke, diabetes, reflux disease and impotence.
To evaluate where you are on the Epworth Sleepiness Scale click here. This measures the range of sleepiness and if you should seek treatment or not.
How do I get tested for sleep apnea?
To get tested there are two types of sleep tests that can be ordered by a medical doctor. Typically pulmonologists, ENT’s and Primary care physician’s or physicians that have a sub specialty in Sleep Medicine can order a polysomnography (PSG) sleep test or a Home sleep test (HST). Once diagnosed with sleep apnea, there are multiple ways to treat sleep apnea.
To help facilitate finding the appropriate doctor for you, we can help. Contact us and we will help direct you!!
How to treat sleep apnea?
There are multiple treatment options for patients to treat sleep apnea. One of the most common causes of sleep apnea is obesity. Maintaining a healthy diet, exercising and having an appropriate Body Mass Index (BMI) will help significantly.
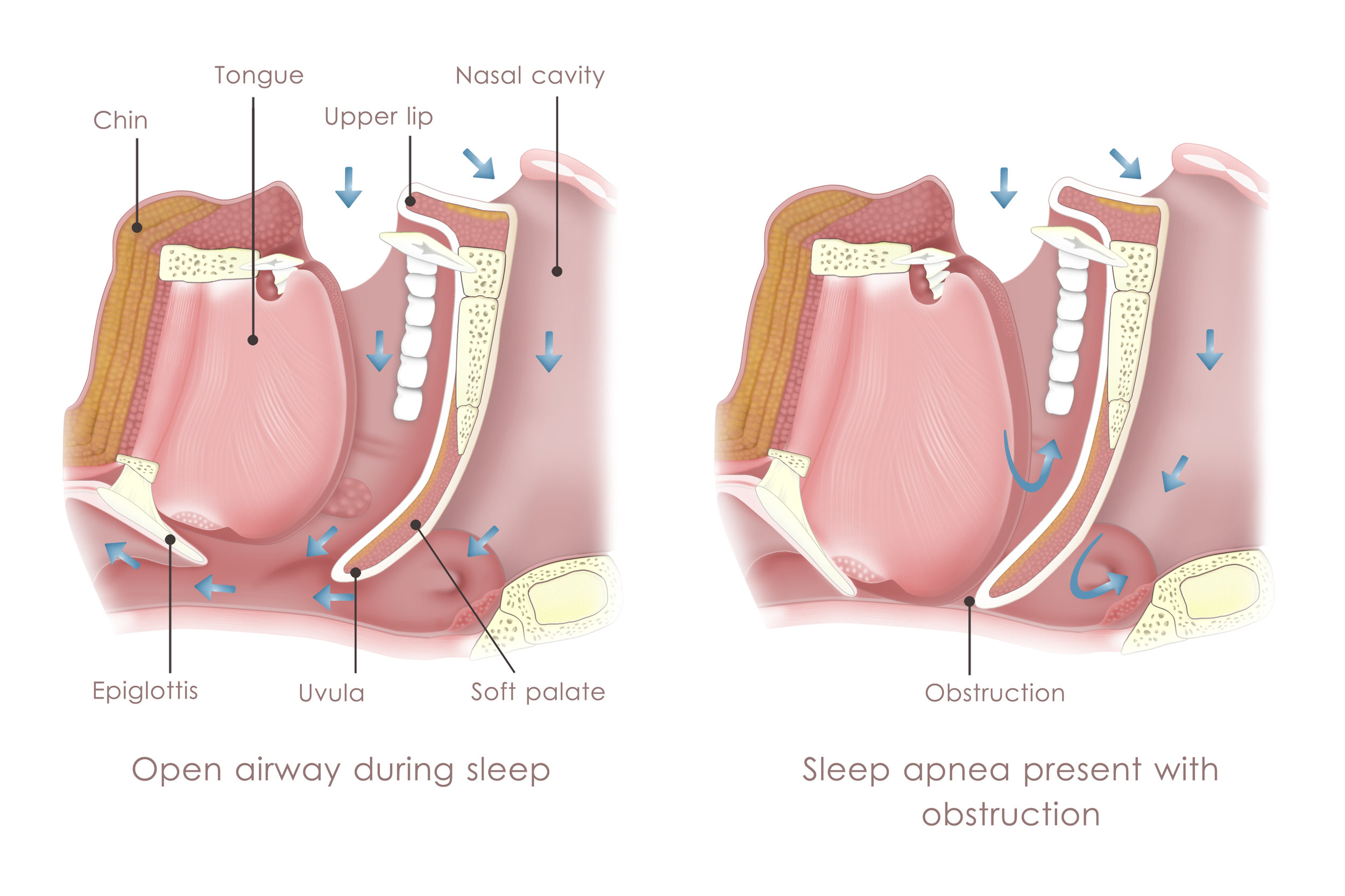
Most sleep physicians will recommend a Continuous Positive Airway Pressure (CPAP) Therapy. CPAP is a airway pressure regulator that applies air pressure on a continuous basis to help maintain the airway open so each person can breath without having an apneic event. CPAP has a mask or nasal pillows that are strapped to the patients head. Some risks to CPAP include the mask or pillows leaking air or inability to have the mask/pillows fitting properly, discomfort with the mask, inability to fall asleep or interrupted sleep to the presence of the device, noise from the device disturbing sleep or the bed partners sleep, CPAP does not seem to be effective, pressure on the upper lip causes tooth related issues, latex allergy, claustrophobic associations or an unconscious need to remove the CPAP at night.
The most drastic option is surgery. The most common procedure is called Uvulopalatopharyngoplasty (UPPP). This procedures removes the uvula, tonsils, adenoids and a portion of the soft palate to help reposition and remodel the soft tissue to allow for a larger area for air to flow. The other surgical option is the Inspire therapy where they place an implant to help but you have to be a candidate for this and they have strict guidelines.
Oral appliance therapy (OAT) is an alternative treatment option to CPAP, surgery or doing nothing. This is what we focus on. We make an oral appliance to reposition the patients jaw forward (Mandibular advancement device) allowing the tongue to move forward and increase the volumetric area for air to travel.